Q. Can you guess which part of the body this medical object was used for?
Face
Knee
Ear
Have a closer look at the 3D image, spin it around.
Can you work out what material it’s made from?
How old do you think it might be? When do you think it was made?
Can you spot any moving parts? Try clicking on the ‘Close’ and ‘Open’ buttons…
It is about the size of an adult hand.
To investigate our object in a 3D visualisation, please use the Google Chrome browser.
FACTS
Pain was a major problem in surgery, it resulted in surgeons like Robert Liston becoming fast and, ultimately, experts in certain procedures. Even so, surgery remained a last resort and internal medicine was never attempted.
Three barriers to surgery which challenged surgeons and patients were:
Pain
Blood loss
Infection
Everybody feels pain. You may have recently stubbed your toe or banged an elbow against the door and had a jolt from your body telling you that was a silly thing to do!
Q. What might happen to a patient in the 1840s experiencing pain?
They might:
Not pay their medical bill because of the experience,
Move and squirm around making it harder for the surgeon to complete the operation,
Pass out or die from shock,
Scream and shout making hospitals a difficult place to work or visit, or
Experience the fight or flight in response to the pain and injure the surgeon.
Well, you might not believe it but apart from 1., all of these would be possible. Surgeons could even ask for their fee upfront due to the 1 in 4 chance of the patient dying either during or after a procedure.
Pain during surgery was intense and surgeons worked hard to develop techniques to ensure they were quick. They also tried hard to ensure at least some pain relief for the patient, even if this was only a very simple distraction technique. Pain-free surgery was easier for the surgeon, too!
Common Surgery Procedures 1800-1850
Q. so How did this mask help with the pain of surgery in the 1800S?
Q. Have you guessed what this mask is for, yet?
It is a Schimmelbusch mask, and was used to deliver primitive anaesthetics to patients, providing pain relief for the purposes of surgery. Curt Schimmelbusch invented this mask in around 1889 and we know that this type of mask, and earlier forms of anaesthetic masks, would have been used in the Worcester Infirmary on Castle Street for many decades.
fact
Anaesthetic was a welcome addition to medical care when it finally arrived in 1846.
a quick history of anaesthetics
Check out this short timeline for a few facts about ether.
“ …seemed capable of destroying pain and might probably be used with advantage in surgical operations... ”
However, he did nothing more with that thought!
1815 Michael Faraday noted similar effects in ether and the entertainment from ‘ether frolics’ began. These ‘frolics’ included inhaling ether to give a giddy feeling or to pass out for fun!
1835 Jean-Baptiste Dumas identified chloroform but did not specify what it might be used for.
1842 Crawford Long (1815-1878) a doctor in Jefferson, Georgia, USA had experienced ‘ether frolics’ and noticed he never felt any pain when he had bumped himself during the parties. He began to use it for his practice, firstly removing a tumour from a boys neck. Long did not publish his work until 1849 and is often forgotten about, even though he was the first to use anaesthetic for medical purposes.
1844 Horace Wells (1815-1848) a dentist in Hartford, Connecticut, USA watched a public exhibition by travelling showman ‘Professor’ Gardner Quincy Colton involving ‘laughing gas’ and noticed the ‘tester’ banged his leg but didn’t even flinch! Wells asked his colleague dentist to remove his healthy molar after he had taken the nitrous oxide. Wells woke up with one less molar and no knowledge or pain from the extraction. Wells promoted a public demonstration but it didn’t go well. He lost his confidence, didn’t recover and committed suicide some years later.
1846 Wells’ dental partner William Thomas Morton (1819-1868) also saw the potential benefits of pain-free operations. He moved to Boston to research and was told about ether by Dr Charles Jackson. In October 1846 Morton persuaded surgeon John Collins Warren to try it with a patient and it was successful.
Morton tried to make his fortune by changing the ether’s colour and renaming it to avoid competition. It backfired because it was soon discovered to be ether! When the US Government acknowledged that a $100,000 reward was due to the person who introduced anaesthetic for pain-free surgery they could not decide who was most worthy - Wells, Morton or Long.
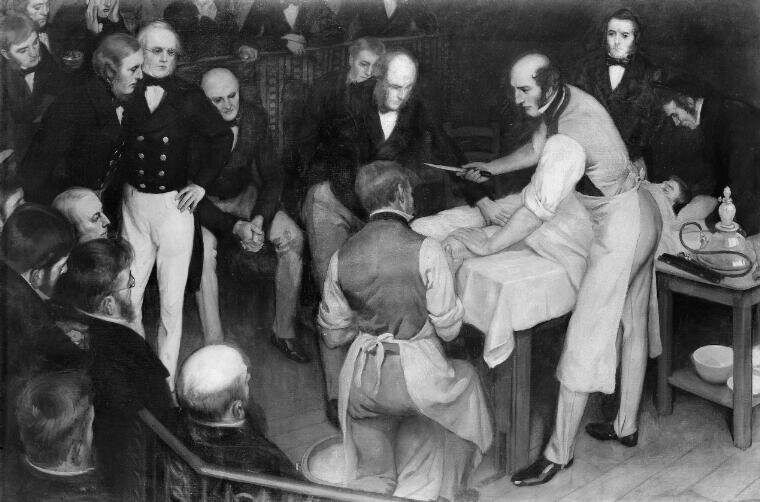
1846 December 21st, ether was reintroduced into the scientific forum in London, as Robert Liston put his patient under anaesthetic calling it the ‘Yankee dodge’. The patient awoke after having the lower leg removed and he knew nothing about it! A success!
Credit: Robert Liston operating. The artist was Ernest Board of Bristol (1877-1934), and this was one of the paintings he was commissioned to paint by Henry S. Wellcome circa 1912. Credit: Wellcome Collection. Attribution 4.0 International (CC BY 4.0)
Such a development created a shift in ideas and a huge benefit for both patient and surgeon, as the patient was more likely to be still for longer as they felt no pain.
However, there were also some downsides to ether:
It is highly flammable,
Ether is difficult to administer safely for the patient,
Surgeons took advantage of the patient no longer squirming and would have more of a look around while wounds were open. There is a saying that ‘the operation was a success, but the patient died’ - many patients died due to being ‘under’ the effects of anaesthetic for too long, or from infection. Either way, the death rate rose.
fact
Check out this short history of chloroform and James Young Simpson.
Q. Who was Sir James young simpson?
Professor of Midwifery and Obstetrics at Edinburgh University, Sir James Young Simpson was a hugely respected physician and is credited with introducing chloroform, rather than ether, for childbirth and other surgical procedures. He was informed about its benefits by a Manchester chemist and experimented on himself and his friends to perfect the portions required.
Chloroform (CHCl3) is a dense, clear and colourless liquid which evaporates. It releases toxic fumes as it decomposes.
In terms of its qualities verses ether, it could be used in smaller quantities, it was quicker to work on patients, less expensive and easier to transport. It needed no special apparatus and could be dropped onto a sponge to deliver results simply. Unlike ether, chloroform is also not flammable, although it could cause a rash if it was accidentally dropped on the skin. So, anaesthetic masks like the Schimmelbusch mask were designed to deliver the chloroform safely (see the gutter in the film - designed to capture any excess liquid).
People weren’t entirely sure about using chloroform in childbirth until John Snow was permitted to use it in 1853 on Queen Victoria as she gave birth to her eighth child, Prince Leopold. After the Queen’s seal of ‘royal approval’, everyone wanted to use it!
It was not until 1937 that the use of chloroform started to decline when Medical research established chloroform placed some patients at risk of cardiac arrest. It can also cause kidney and liver cancer.
Q. was it all Good news?
Image: James Young Simpson unconscious after chloroform experiment
Not all doctors were supportive of the use of chloroform, claiming it violated their professional ethics. Some believed that chloroform ‘seduced’ patients into avoiding pain, helping them pass into a level of consciousness about which little was known. Others stated it risked a patient being interfered with sexually whilst unconscious.
A religious argument was also used against administering chloroform during childbirth, claiming that God ordained women to suffer during childbirth and chloroform prevented it. They quoted from the Book of Genesis: “To the woman he said, I will greatly increase your pains in childbearing; with pain you will give birth to children. Your desire will be for your husband, and he will rule over you.”
Simpson responded saying that anaesthetics came from God "…so the Lord God caused man to fall into a deep sleep; and while he was sleeping he took one of man's ribs and closed the place with flesh." He also quoted the Book of James chapter 4 verse 17, “If anyone, then, knows the good they ought to do and doesn't do it, it is sin for them.”
Funded by West Midlands Museum Development with Art Fund support